World Physical Therapy Day 2024 is on Sunday, September 8, 2024: what is the difference between an occupational therapist and a physical therapist?
Sunday, September 8, 2024 is World Physical Therapy Day 2024. Physical Therapists Outpatient Rehab Locations in Delco, Chesco and Montco. More Info
As an Amazon Associate I earn from qualifying purchases.

The human body is remarkably simple to damages and break, and no more so compared to when participating in exhausting exercise such as sporting or athletic task.
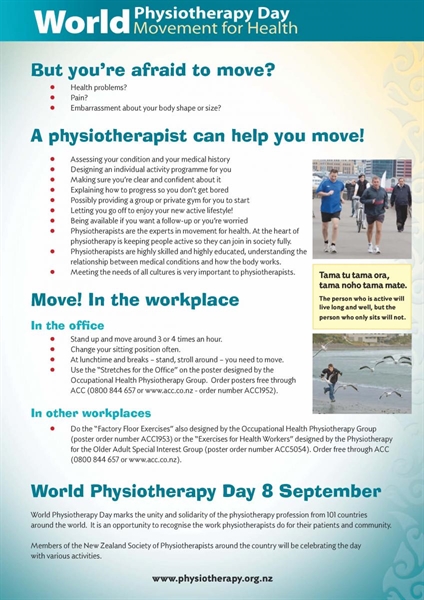
Physiotherapists work to reverse damage, inform on healthy and balanced behavior and to restore lost or ruined capability. Bodily Therapy Day, then, is devoted to these specialists throughout the globe, and aims to acknowledge their commitment to keeping us all fighting-fit.
Occupational Therapy:
According to the World Federation of Occupational Therapists, Occupational Therapy (OT) is defined as a profession concerned with promoting health and well being through occupation. There is a definite process that is followed by occupational therapists. It is called the Occupational Therapy Process. The stages of this process are referral, information gathering, initial assessment, requires problem identification, goal setting, action planning, ongoing assessment and revision of action, outcome and outcome measurement, end of intervention or discharge and review. Occupational Therapy is widely used in physical, mental and community health settings.
Physical Therapy:
Physical Therapy (PT) is concerned with providing services, where functions and movements are hampered by injury, disease, or environmental factors. It covers physical, social, psychological and emotional well being of an individual. Physical therapy is used to give maximum mobility and functional ability throughout the life of a person. Basically, it involves focusing on a specific part, which has undergone trauma, for example a fracture or a torn ligament and giving it certain kind of exercises. In the early days of physical therapy, it was only restricted to exercise, massage and traction.
Check out the Department of Labor and Statistics as well as descriptions change year to year.
~Best Wishes!!!
cognitive behavioural therapy?
What is CBT?
It is a way of talking about:
How you think about yourself, the world and other people
How what you do affects your thoughts and feelings.
CBT can help you to change how you think ("Cognitive") and what you do ("Behaviour)". These changes can help you to feel better. Unlike some of the other talking treatments, it focuses on the "here and now" problems and difficulties. Instead of focussing on the causes of your distress or symptoms in the past, it looks for ways to improve your state of mind now.
It has been found to be helpful in:
Anxiety
Depression
Panic
Agoraphobia and other phobias
Social phobia
Bulimia
Obsessive compulsive disorder
Post traumatic stress disorder
Schizophrenia
How does it work?
CBT can help you to make sense of overwhelming problems by breaking them down into smaller parts. This makes it easier to see how they are connected and how they affect you. These parts are:
A Situation - a problem, event or difficult situation
From this can follow:
Thoughts
Emotions
Physical feelings
Actions
Each of these areas can affect the others. How you think about a problem can affect how you feel physically and emotionally. It can also alter what you do about it.
What does CBT involve?
The sessions
CBT can be done individually or with a group of people. It can also be done from a self-help book or computer programme. In England and Wales two computer-based programmes have been approved for use by the NHS. Fear Fighter is for people with phobias or panic attacks, Beating the Blues is for
people with mild to moderate depression.
If you have individual therapy:
You will usually meet with a therapist for between 5 and 20, weekly, or fortnightly, sessions. Each session will last between 30 and 60 minutes.
In the first 2-4 sessions, the therapist will check that you can use this sort of treatment and you will check that you feel comfortable with it.
The therapist will also ask you questions about your past life and background. Although CBT concentrates on the here and now, at times you may need to talk about the past to understand how it is affecting you now.
You decide what you want to deal with in the short, medium and long term.
You and the therapist will usually start by agreeing on what to discuss that day.
With the therapist, you break each problem down into its separate parts, as in the example above. To help this process, your therapist may ask you to keep a diary. This will help you to identify your individual patterns of thoughts, emotions, bodily feelings and actions.
Together you will look at your thoughts, feelings and behaviours to work out:
- if they are unrealistic or unhelpful
- how they affect each other, and you.
The therapist will then help you to work out how to change unhelpful thoughts and behaviours
It's easy to talk about doing something, much harder to actually do it. So, after you have identified what you can change, your therapist will recommend "homework" - you practise these changes in your everyday life. Depending on the situation, you might start to:
Question a self-critical or upsetting thought and replace it with a positive (and more realistic) one that you have developed in CBT
recognise that you are about to do something that will make you feel worse and, instead, do something more helpful.
At each meeting you discuss how you've got on since the last session. Your therapist can help with suggestions if any of the tasks seem too hard or don't seem to be helping.
They will not ask you to do things you don't want to do - you decide the pace of the treatment and what you will and won't try. The strength of CBT is that you can continue to practise and develop your skills even after the sessions have finished. This makes it less likely that your symptoms or problems will return.
![]()
What is music therapy...?
Music therapists use music creatively to help their clients address social, emotional or physical problems. They work with a variety of clients of all ages and social backgrounds and in a variety of settings.
Music therapists seek to establish an interaction - a shared musical experience - in the pursuit of therapeutic goals. These goals are determined by the therapist's understanding of the client's pathology and personal needs. Music therapists support clients with a wide range of problems, which may include eating disorders, anxiety, behavioural problems, stress management, and dealing with the effects of abuse.
Music therapy is based on the development of a relationship between the therapist and client, who communicate through music-making, either in groups or on a one-to-one basis.
Typical work activities include:
* agreeing objectives of the therapy with the client at the outset of the relationship;
* recording therapy sessions, with the consent of the client(s);
* reviewing and assessing therapy sessions afterwards to monitor effectiveness and to aid the planning of subsequent sessions;
* taking an active role in sessions by playing, singing and listening;
* encouraging clients to take part in the session, and supporting them by responding musically;
* encouraging clients to use musical instruments, such as percussion and voice, to express themselves;
* helping clients explore the world of sound and to create a musical language of their own;
* improvising with music as a reaction to what the client is communicating;
* facilitating positive changes in the behaviour and wellbeing of the client, encouraging non-verbal communication.
Additional work activities include:
* planning and reviewing each session;
* assessing the musical and non-musical behaviours of the client;
* writing up case notes and reports.
Music therapists working in a clinical setting may spend a high percentage of their day liaising with medical colleagues and other professionals engaged in the care of their clients. In other settings, for example when clients have referred themselves or their children, therapists may take a less formal approach to reporting back the client's progress.